COVID-19 & Healthcare Workers
Prepared for Service Employees in International Union-United Healthcare Workers West
The COVID-19 pandemic changed the rules of labor for almost everyone. For those who toil in frontline, essential jobs, the impact has been significant as the virus upended workers' health, employment, hours, and pay. Many of these workers lack health insurance, paid time off or the most basic rights in the workplace—rights that others take for granted.
In California, the Service Employees International Union-United Healthcare Workers West (SEIU-UHW) represents more than 100,000 people employed by healthcare organizations. Members include janitors, respiratory therapists, caregivers, environmental service technicians who handle bio-hazardous waste and others who perform direct and indirect patient care.
This research project aims to figure out if workplace conditions and on-the-job changes during the pandemic make healthcare workers more likely to become ill with COVID-19. To collect information about their working conditions, we asked SEIU-UHW members to take the COVID-19 Survey for Workers. SEIU-UHW reached out three times with information on the survey and how to access it. Members took the online survey between June and August 2021, after vaccinations had become widely available and during the period when the Delta variant was surging.
Research Takeaways
Long before the COVID-19 pandemic, health scientists understood that stress on the job can have a negative impact on workers’ health. This is particularly well documented among healthcare workers. Previous research also reveals that low job control, high environmental stress and low household income have a cumulative effect on health.
In our study, most healthcare workers who took the survey were in a state of vigilance as the Delta variant raged around them and they believed the risk of COVID-19 exposure at work was significant, even when they tested negative for the virus.
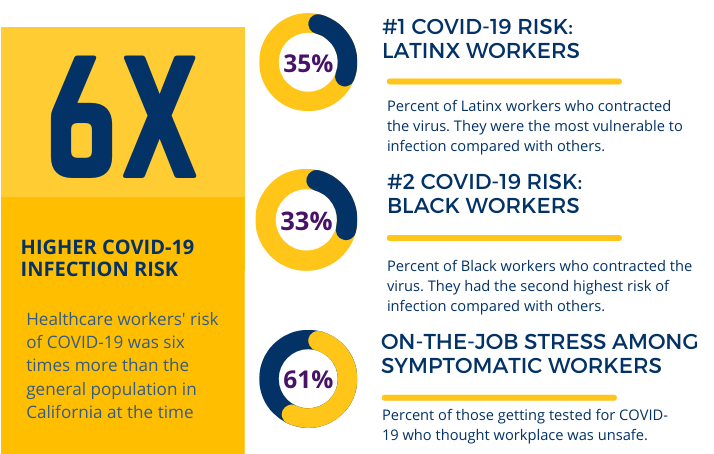
Our survey data confirmed a basis for these concerns. Overall, healthcare workers had a much higher risk of getting sick with COVID-19. Those who took the survey were six times more likely to have been affected at some point than the general population, even as these same healthcare workers had high rates of vaccination (83%). Among those who did test positive for COVID-19, more than three-fourths (77%) attributed illness to exposure at work.
Numbers and Statistics
The COVID-19 Survey for Workers collected data from 421 frontline healthcare workers during the emergence of the Delta variant in California when cases and deaths were increasing and vaccines had been available to frontline workers for several months.
The Physical and Emotional Impact
- 32% were diagnosed with Covid-19. Nearly 1 in 3 frontline SEIU-UHW healthcare workers had been told by a healthcare provider they had COVID-19, compared with 5% of Californians.
- 55% knew someone who had died due to Covid-19. Of those who knew someone who died, 80% lost at least one friend or close relative.
- 72% had fear and anxiety. Almost three-quarters of workers were worried about family or others getting COVID-19.
- 55% couldn't sleep. Workers had difficulty falling or staying asleep often or very often.
- 45% said they were in a daze. Workers felt not their usual self often or very often.
- 52% felt disconnected from others. Workers felt that they were losing touch with friends often or very often.
The Economic Impact
- 13% had no paid sick leave. Either their employer did not provide sick leave or they had used up their sick leave. An additional 33% needed to take more sick days than they had available.
- 43% had to take time off. 23% of all survey participants lost a week or more of work. Time taken off ranged from 1 to 120 days.
SEIU-UHW Member Statistics
Out of the 421 total survey participants, 36 percent of respondents did not provide their race or ethnicity. Among those who did, 80% were female and 48% were Latinx—which is typical for California’s allied healthcare workforce. This differs from SEIU-UHW’s membership which are 51% female, 21% male, and 28% unknown sex. Furthermore, SEIU-UHW’s membership, among those who provided race and/or ethnicity is: 32% Latinx, 25% Asian/Pacific Islander, 22% White/Caucasian, 12% Black/African American, 9% multi-racial, and a very small fraction are American Indian / Alaska Natives.
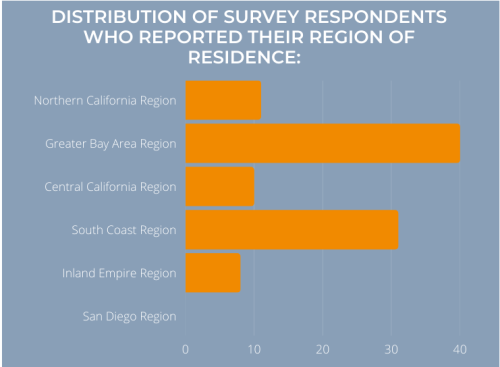
Out of the 421 participants that answered the survey, 255 members answered which California county they reside in. Participants resided in five of the six regions in California: Northern California, Central California, Greater Bay Area, South Coast, and Inland Empire. After excluding SEIU-UHW members outside of California, then limited to those whose county of residence was known, respondents to the survey were distributed geographically similar to the SEIU-UHW membership for all six regions in California, with the exception that there was a higher percentage from the Greater Bay Area among survey respondents: 40% versus the 33% of the SEIU-UHW membership.
SEIU-UHW Members and Their Jobs
There were a total of 331 job titles reported amongst the 421 survey participants:
- 84.7% work in health, healthcare, or pharmacy
- 6.8% self-employed, private homes, or other
- 3.5% supermarket or grocery stores, other retail, restaurants, eating and drinking places. (e.g. coffee shops, bars, breweries),hotels, or hospitality
- 0.9% Manufacturing, wholesale or distribution
- 0.9% Scientific, technical, and education
- 6.3% Did not answer or preferred not to answer
- 3.4% transportation of people, government, public administration (other than finance), or Services (not otherwise listed)
Percentages add up to more than 100% because some participants worked more than one job and in different industries.
PPE Provided by Workers vs. Employers
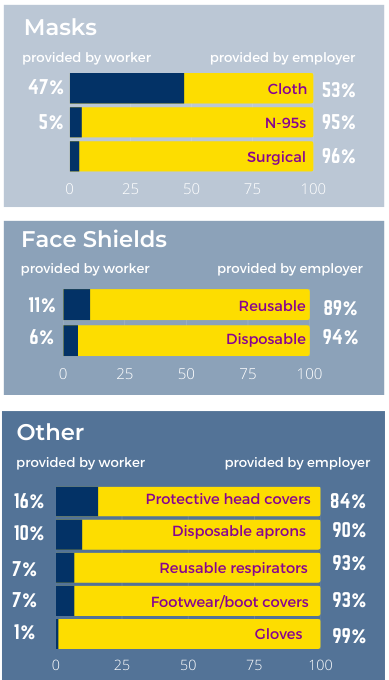
“I bought my own surgical masks most of the pandemic since my employer was not willing to buy different sizes.” —SEIU-UHW member
During the early period of the pandemic, many employers did not implement workplace rules that could have better-protected employees and patients. Half of those surveyed reported their employers required the reuse of disposable masks, and some employers provided workers with masks used by others.
NIOSH-certified N95 respirators are designed to be single-use devices and filter 95% of particles when appropriately fitted. This means that an N95 that's not properly fitted likely gives the wearer less protection.
Employer Practices
About 1 in 5 respondents worked for an employer who, at some point during the pandemic, started decontaminating disposable masks or respirators. Very few of the respondents (7%) worked for an employer that mandated rapid COVID-19 testing before work. Of the 306 respondents working at the time of the survey:
- 5% reported that they were provided with a mask that others had worn
- 20% reported that they worked for an employer that decontaminated disposable masks or respirators to make them last longer
- 51% reported that they were required by their employer at some point during the pandemic to reuse masks meant to be disposable
- 64% reported that their employer never conducted fit testing of respirators
Survey respondents reported a lack of the following practices in one or more of their jobs during the pandemic:
- 19% No body temperature checks for employees
- 44% No additional stations/supplies for sanitizing hands
- 48% No distancing among workers, or between workers and clients
- 53% No physical barriers between workers and others
- 93% No rapid COVID-19 testing before work
A large majority of respondents (86%) had at least one employer during the pandemic who required temperature checks, but 14% had no employer who required temperature checks. The 41% without additional hand sanitizing supplies may simply reflect that their healthcare employers already had those stations widely available.
Slightly more than half of respondents worked for at least one employer during the pandemic who physically distanced staff from each other or from patrons/clients. However, 46% did not, in any of their jobs during the pandemic, have an employer who physically distanced the workers.
About half (51.3%) of the respondents labored for employers who did not add any type of physical barriers between workers and others.
Employer Differences: Infection Rates and Job Types
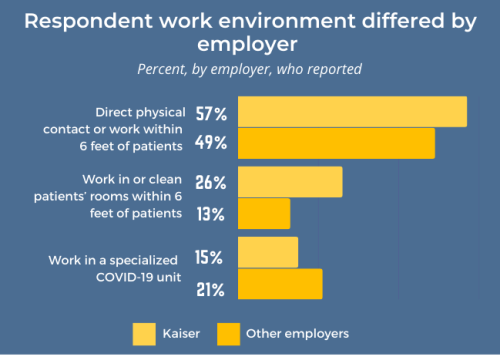
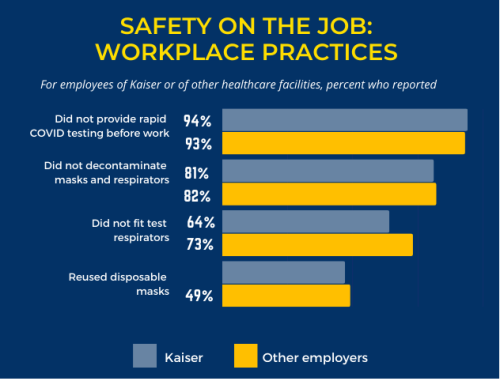
53% of SEIU-UHW members work for Kaiser Permanente, while 47% work for other hospitals. For virtually every safety measure, Kaiser was similar to other healthcare providers in supplying head covers, N-95 masks, gloves, decontaminated PPE, and testing before work. However, employees of Kaiser Permanente were more likely to work in jobs having physical contact with patients or cleaning patients’ rooms (see graph above).
About two-thirds or more of all employers did not fit test respirators. Close to half of respondents employed either by Kaiser or by other facilities were required at some point during the pandemic to reuse disposable masks.
No one is safe unless we all are, so why aren't all healthcare workers protected?
The fact is, protecting workers is as much a health and safety issue for them as it is for the patients they care for. Frontline healthcare workers who get sick can't help COVID-19 patients get healthy. As long as the pandemic continues cycling between surges and relative lulls, vulnerable workers remain at risk. We're all in danger.
The virus is now thriving in both vaccinated and unvaccinated people, and with time, immunity is waning in the inoculated or infected. As the Omicron variants have shown us, SARS-CoV-2 mutates easily and can become more transmissible. With multiple new variants, vigilance is critical. Increasing booster rates can reduce transmission and severity of disease. Everyone must do their part to finally put this pandemic to rest.
In the meantime, employers are responsible for providing safe working environments. Key steps to protect frontline workers most at risk for COVID-19 exposure include the following:
Recommendations
- Providing free COVID-19 tests
- Requiring physical distancing—to the extent possible—in workplaces
- Providing N95 masks that adequately fit each employee
- Offering easily accessible information on COVID-19 workplace policies and procedures
- Reporting COVID-19 illness or death in a timely manner aligned with current CDPH guidelines to potentially exposed workers
- Implementing CDC and CDPH guidelines and protocols for COVID-19 prevention
-
Extending sick leave to incentive not returning to work while still infectious
Workers' Voices
“My employer handled the pandemic horribly. Very little communication, no consistency in mask mandates and expecting employees to come to work despite being symptomatic and exposed.”
"The frontline workers exposed to the virus the most are the ones who make less money. Many times, I’ve thought of leaving my job."
“I'm sure I contracted COVID from work. Healthcare workers were not given proper PPE for a very long period of time! We passed the virus around, many of us purchased our own PPE and were never encouraged to get tested or stay home."
"My employer refused to provide PPE. They took all of our masks, gloves, hand sanitizers and Clorox wipes, exposing a whole department to COVID-19. The employees were afraid to call in sick due to discipline, therefore they came in and exposed fellow coworkers.”
“There were times we were not provided N-95 masks and asked to double up on surgical masks. We were short plastic gowns and asked to use patient hospital gowns. We provided our own face shields and lab coats due to short supply. We also were cheated out of extra shift and other pay incentives and struggled to keep the lab staffed properly as a result of management's manipulation of pay and lack of communication. Nobody wants to work extra shifts or hours if we have to fight to get paid appropriately. Our department is falling apart due to stress and exertion.”
"Upper management and chiefs received sealed, good boxes, and essential workers working directly with patients received tampered boxes. Employees were working long hours with poor PPE."
"Mask boxes were tampered, torn and musty, and in storage units with insect and rat feces. Employees were becoming ill."
"We had to locate management to get N-95 masks and were asked if the patient was COVID positive. If not, management wouldn't give us an N-95."
"Before COVID-19, PPE was always available. Once it hit, supplies vanished! One-time use supplies were being used multiple times, especially when no more N-95s were available."
"Being a healthcare worker has been hard—going to work not knowing if I would bring anything home to my children.”
SEIU-UHW members gave their testimonies for this report from March 2020-August 2021. Members requested anonymity.
