By Pamela J. Lein, PhD and Anthony S. Wexler, PhD
Human exposure to unhealthy levels of air pollution is now a worldwide public health problem, and in heavily urbanized areas of both developing and developed countries, levels of some air pollutants can exceed safe air quality standards by a factor of 10 or more.
In a 2017 review of the global burden of disease (“The Lancet Commission on Pollution and Health”), polluted air was identified as the predominant cause of pollution-associated morbidity and mortality. A subsequent 2018 World Health Organization (WHO) report estimated that ambient air pollution causes 4.2 million premature deaths per year. While it is widely recognized that air pollution contributes to respiratory and cardiovascular disease, a growing body of evidence has shown that air pollution can also have harmful effects on the brain, especially affecting brain health of children and the elderly.
Air pollutants exist in two phases in the atmosphere: the gas phase and the particle phase. Gaseous pollutants include ozone, nitrogen dioxide (NO2), and a wide range of volatile organic compounds (VOCs).
Particles, also referred to as particulate matter or PM, are microscopic liquid droplets and solid matter in the atmosphere. PM includes biological particles such as pollen, bacteria, viruses, and spores, as well as suspended non-biological solids, such as dust and smoke.
Particles vary considerably in size and composition. The size of ambient PM ranges from coarse (PM10 with an aerodynamic diameter less than 10 µm) to fine (PM2.5, diameter < 2.5 µm) to ultrafine (UFPM or 1 PM0.1, diameter < 0.1 µm). The chemical composition of PM varies considerably based on geographic location, weather, season, time of day, and many other factors, including particle size. The smaller PM fractions typically contain higher amounts of black carbon and other products of incomplete combustion, while PM10 contains more metals, inorganic material, and other debris and dust from mechanical processes (Table 1).

Among the different organic compounds absorbed to PM, of particular concern to brain health are the PAHs, polycyclic aromatic hydrocarbons, which are neurotoxic to the developing brain. Neurotoxic metals and metalloids are also detected in PM, including lead (Pb), manganese (Mn), methyl mercury (MeHg) and arsenic (As).
Air pollution exposures are not restricted to the outdoor environment. Outdoor air pollutants can travel indoors where many people spend most of their time. For example, the typical American spends an average of 90% of his/her time indoors.
It turns out that for many people, the majority of their exposure to outdoor air pollution can actually occur indoors. Cooking and home heating generate PM. VOCs are emitted from building materials, paints and protective coatings, carpeting, furniture, cleaning chemicals and other products. Read more about indoor and outdoor air pollution.
How does air pollution harm the brain?
Research conducted by Lilian Calderόn Garcidueñas in Mexico City more than 15 years ago provided the first experimental evidence linking air pollution to adverse effects on brain health. Her initial studies were of the brains of street dogs. These studies revealed that dogs living in the polluted air of Mexico City exhibited significantly more neuro degeneration than age-matched dogs living in environments with cleaner air outside of Mexico City. Her subsequent studies of children and young adults living in areas with high air pollution identified changes in their brains that resembled the brain pathology observed in patients with Alzheimer’s disease.
Following on the pioneering work of Calderόn Garcidueñas, numerous epidemiological studies of diverse populations in multiple geographical locations have linked air pollution, and in particular traffic-related air pollution and/or PM2.5 levels, to increased risk of neuro degenerative disease. In 2019, six separate meta-analyses/systematic reviews of the epidemiological literature concluded that the data support a strong association between ambient PM2.5 and a wide spectrum of neurological disorders, including age-related dementia, Parkinson’s disease, Alzheimer’s disease, stroke, depression, and anxiety disorders. We also now know that the developing brain of children is susceptible to the adverse effects of air pollution. Epidemiological studies have identified traffic related air pollution, ambient PM2.5 and PAHs as environmental risk factors for neurodevelopmental disorders, in particular autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD).
How is air pollution related to "brain fog"?
A more recent realization is that air pollution not only increases the risk of neurologic disease, but also exerts more subtle effects on the healthy brain – decreased productivity termed “brain fog”. Across multiple occupational sectors ranging from agricultural workers in the fruit orchards of California to indoor workers in the manufacturing sector to white-collar office workers in the service sector, short-term exposure to high levels of outdoor air pollution has been consistently associated with decreased worker output.
Short-term exposure to high levels of outdoor air pollution has been consistently associated with decreased worker output.
For example, an analysis of 10 years of S&P 500 returns as a proxy for job performance of stockbrokers working on the New York Stock Exchange found that higher ambient PM2.5 levels in New York City were associated with reduced stock trading returns. A similar association was reported for more than 100,000 investors at a German brokerage firm. Studies in which pollutant levels were experimentally manipulated confirm that air pollution influences human performance. For example, airline pilots performed better during advanced maneuvers under conditions of lower vs. higher CO2 levels.
Similarly, office workers performed significantly better on cognitive tests when taking the tests in rooms with lower VOC and CO2 levels. Test scores in the low VOC/low CO2 rooms were improved even further when ventilation rates were increased. The authors of this study estimated that increasing building ventilation standards from the current recommended 20 cubic feet per minute per person (cfm/p) to 40 cfm/p would cost $40 per person in energy expenditures, but companies would gain $6,500 per employee from greater productivity.
How does air pollution affect children?
Recent studies in Barcelona, Spain suggest that air pollution also causes brain fog in children. Increases in daily ambient levels of traffic-related air pollution were associated with reduced attention spans amongst children in elementary school. In Israel, higher daily PM2.5 levels were associated with reduced performance by high school students on college admission exams. Follow-up studies of subjects at 28-30 years of age indicated that higher exam-day PM2.5 levels were associated with fewer years of post-secondary education and reduced monthly earnings.
Increases in daily ambient levels of traffic-related air pollution were associated with reduced attention spans amongst children in elementary school.
The effects of air pollution on cognitive function in otherwise healthy individuals appear to worsen with increasing duration of exposure. A recent study in China that examined a nationally representative sample of more than 25,000 children and adults in 162 counties found that the negative impact of a higher air pollution index on cognitive function was significantly greater for long-term (up to 3 years) exposure compared to short-term (1-7 day) exposure. Similarly, higher PM2.5 exposure in Southern California is associated with reduced intelligence in adolescents and young adults with stronger associations observed in males and individuals of lower socioeconomic status.
While epidemiological studies can identify associations between air pollution and altered brain function or disease, they cannot establish a cause-effect relationship. Corroboration of human findings in experimental models are often required to address the question of causality. A number of experimental animal studies have shown that controlled exposure to concentrated ambient particles or to diesel exhaust causes both behavioral and pathological changes in the brain that are relevant to human neurodevelopmental disorders and neurodegenerative diseases. Studies using cultured cells derived from human brain tissues also support a causal relationship between PM2.5 and outcomes associated with neurological disease.
How does air pollution alter brain development and function?
Magnetic resonance imaging (MRI) studies in humans reveal that increased exposure to PM2.5 is associated with changes in brain structure in older adults, including brain atrophy. These changes occur prior to the appearance of dementia. Similar changes in brain structure occur in laboratory animals exposed to air pollution. Experimental animal studies further show that air pollution triggers inflammation and oxidative stress in the brain. Both inflammation and oxidative stress are implicated in the pathogenesis of neurodevelopmental disorders, anxiety and depression, and neurodegenerative diseases, 5 PM Inhalation PM0.1 PM2.5 PM10 Blood stream.
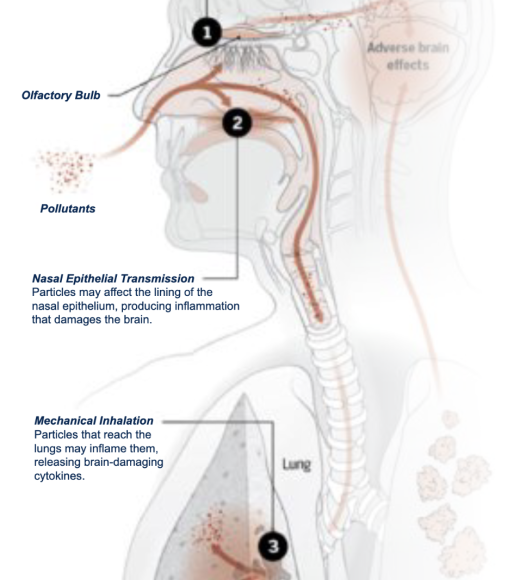
But what gets into the brain after inhalation of air pollutants and how it gets there remain outstanding questions. Experimental studies suggest two possible models of PM translocation to the brain (Figure 1).

In the first model, olfactory nerve endings in the nasal cavity take up or engulf ultrafine PM (PM0.1), which is then transported within the nerve fiber to the olfactory bulb in the brain. In the second model, inhaled PM2.5 reaches the lower airways where it can be transferred to the bloodstream and then distributed to all organ systems of the body, including the brain. Once in the brain, the particles may cause brain damage via multiple, likely overlapping mechanisms:
(a) The physical structure of the particle can activate resident immune cells to trigger neuroinflammation and/or oxidative stress.
(b) The release of neurotoxic chemicals from the particle may directly affect cells in the brain, such as neurons and microglia.
However, other researchers believe that indirect mechanisms mediate the effects of air pollutants on brain health. For example, it is widely accepted that air pollution causes cardiovascular disease, and cardiovascular disease is a significant risk factor for Alzheimer’s disease and age-related dementia.
Thus, it has been proposed that air pollution effects on brain health are the consequence of air pollution-induced cardiovascular disease. While this may contribute to the neurodegenerative effects of air pollution, it seems unlikely to be a major mechanism by which air pollution causes brain fog in health adults or increases risk of neurodevelopmental disorders in children. A second indirect mechanism involves the “lungbrain axis”.
In this model, inflammatory mediators, such as pro-inflammatory cytokines, generated in the lung in response to inhaled PM are transported to the brain via the circulatory system to cause dysfunction and disease (Figure 2).
Where is research headed?
Epidemiologic studies have identified a number neurological diseases associated with air pollution. But significant questions still remain: Is the association causal or is there another intervening factor, such as traffic related noise or socioeconomic status, that underlies the observed association? What are the cellular and molecular mechanisms linking air pollution exposure to altered brain function and disease? What factors influence individual susceptibility to the neurotoxic effects of air pollution?
For example, APOe4 is a known genetic risk factor for Alzheimer’s disease, and amongst women exposed to high PM2.5 levels, those who carry the APOe4 allele are more likely to develop Alzheimer’s disease than those who do not. What other genetic risk factors, or lifestyle factors, modify risk? Which components of air pollution are responsible for the adverse effects on brain health? Gases? Particles? Which ones? Most importantly, what are the sources of neurotoxic air pollution since it is the source that we can control?
While the jury is still out on all these questions, many researchers are focused on PM as the culprit. Of the three categories of components that make up PM:
- Solid inclusions, such as soot or roadway dust
- Water-soluble compounds such as the electrolytes ammonium sulfate or nitrate
- Lipid soluble compounds such as polycyclic aromatic hydrocarbons
The electrolytes are not likely to cause adverse health impacts because the human body is full of electrolytes. The solid inclusions may not be harmful in themselves but the immune system may react to their presence causing inflammation and concomitant health outcomes. The lipid soluble compounds can readily interact with, and modify, biological systems.
As demonstrated by recent work comparing the pulmonary toxicity of particles collected in northern China versus those collected in Sacramento, California, answering these questions will likely not be straightforward. While the particle concentration in air is frequently 3 to 5 times higher in northern China than in Sacramento on a volume basis, the particles collected in Sacramento were more toxic than particles collected in China on a particle mass basis. So why are the Sacramento particles more toxic on a particle mass basis? The answer is not yet known but one hypothesis is that the electrolytes in the particles do not pose a direct health hazard but they dilute the concentration of the toxic components.
Emissions of NOx and sulfur form nitric and sulfuric acids in the atmosphere that then combine with ammonia to condense onto particles as the electrolytes ammonium nitrate and ammonium sulfate. The concentrations of these electrolytes used to be high in the US, as they are now in China, but emissions controls have reduced these concentrations in the US, which may have paradoxically increased the concentration of toxic components in particles.
Answering these questions will require experimental models. However, a major caveat of most experimental studies published thus far is that they have used PM2.5 or diesel exhaust concentrations that are many fold higher than most human exposures and /or employed exposure paradigms that do not capture the complexity or spatiotemporal dynamics of real-world air pollution exposures. Since dose, composition, and timing of air pollution exposures can influence biological outcomes, translating the relevance of much of the published animal literature to the human condition is challenging. The path forward involves developing exposure models that more faithfully replicate human exposures to air pollution.
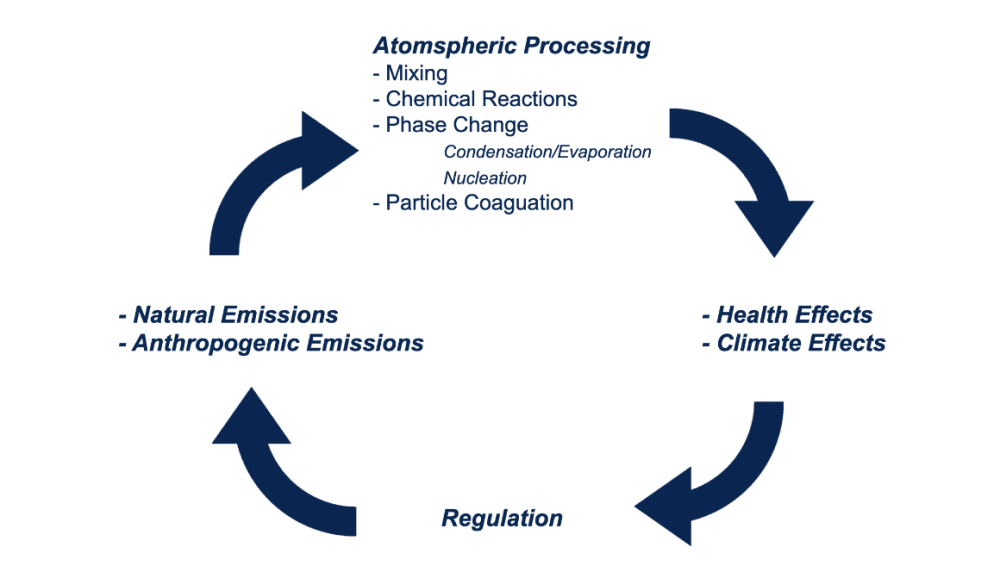
Significant research resources will be needed to address questions of how and which air pollutants adversely affect brain health. Brain dysfunction and disease exact tremendous costs on the affected individual, their families and society. In lieu of curing brain disease, the most expedient and potentially actionable course to curb the predicted increase in a number of brain diseases, such as Alzheimer’s disease, is to identify and limit major risk factors for the disease. Ambient air pollution represents a potential risk factor that could be changed by public policy (See Figure 3 – air pollution life cycle).
While the individual risk of brain disease associated with air pollution may be modest, air pollution may nevertheless result in a significant increase in disease burden because it affects large numbers of people. Reducing air pollution is clearly feasible, but will require compelling evidence of a cause-effect relationship between air pollution and neurological disease to motivate policy and law makers to change standards, as well as the identification of the sources of neurotoxic air pollution that can be controlled by regulation.
Pamela J. Lein is Professor of Neurotoxicology at the School of Veterinary Medicine, University of California, Davis. Anthony S. Wexler is Distinguished Professor of the Department of Mechanical and Aerospace Engineering and Director of the Air Quality Research Center at the University of California, Davis.
This article is an adaptation of the eBook Air Pollution and Brain Health.
